Despite the advances made in treatment and care over the past few decades, ADHD often remains poorly understood. It’s not hard to see why. ADHD is a complex disorder with symptoms that may present differently between genders and coexist with other mental health disorders. That’s not to mention the stigma and cultural bias which must be tackled for patients to receive their diagnosis and necessary treatment.
Despite developments of safe, effective, and evidence-based treatments for children and adults, many challenges and opportunities for change remain. It is the main reason a group of experts in ADHD such as psychiatrists, neurologists, developmental pediatricians, nurse practitioners, psychologists, neuropsychologists, and patient advocates gathered earlier this year to form the ADHD Expert Consortium and published the consensus statement. It gives a comprehensive vision for the path forward utilizing objective data and addressing contemporary challenges in healthcare, particularly ADHD.
In this blog, Danielle Vaeth, senior market manager at QbTech, shares her thoughts on key calls to action and echoes the voices of ADHD experts and patient advocates regarding the much-needed change in ADHD care in the United States.
The need for change
Earlier this year, I hosted an in-person ADHD Expert Consortium to discuss ADHD care. The small group of clinicians and advocates provided their perspectives, which included the impact ADHD has on the public school system.
The most agreed-upon concept mentioned is that ADHD is complex. I am not a clinician. But in the interactions I have had with providers and leaders on this topic, I have also believed this to be true. And yet, over the last decade, I believe there is a large contingent of providers who have felt that it is rarely complex.
For instance, looking at certain guidelines, it has been stated that ADHD should be diagnosed and managed within primary care. Many state best practices include treating ADHD with medication, behavior modification, psychosocial treatments, and managing a chronic condition. What I heard over our meeting and from primary care providers over the past decade is that ADHD symptoms are not straightforward. There are environmental, social, academic, and other physical and mental health factors that are to be considered. All these factors lead to the complexity of ADHD.
Challenges we face
According to statistics and various pieces of literature, there are far too many invisible challenges that children and adults with ADHD face today, such as:
- 90% of individuals with ADHD will continue to have some elevated symptoms throughout their lifetime (only 10% achieve stable remission)
- Children with ADHD have increased accidents and injuries and untreated ADHD adults have more car accidents and injuries than those on treatment
- Mortality rates are significantly increased in individuals with ADHD (accidents, injuries, suicide)
- Those with ADHD are three to five times more at risk for suicide
- Children and adults with ADHD have increased rates of depression, anxiety, substance abuse, and other coexisting conditions. 60-100% have more than one coexisting condition
- Incremental direct medical costs are double for children with ADHD, with an estimated total of $3.921 billion in the US child population
- Indirect costs and burden to families have been calculated to be five times that of the total financial burden of the controls
- Lifetime economic costs of ADHD are substantial: $266 billion annually in 2010 compared to $215 billion for Alzheimer’s Disease in the U.S
- ADHD must be viewed as a public health problem producing a substantial impact on the health, quality of life, and economic viability of the US population
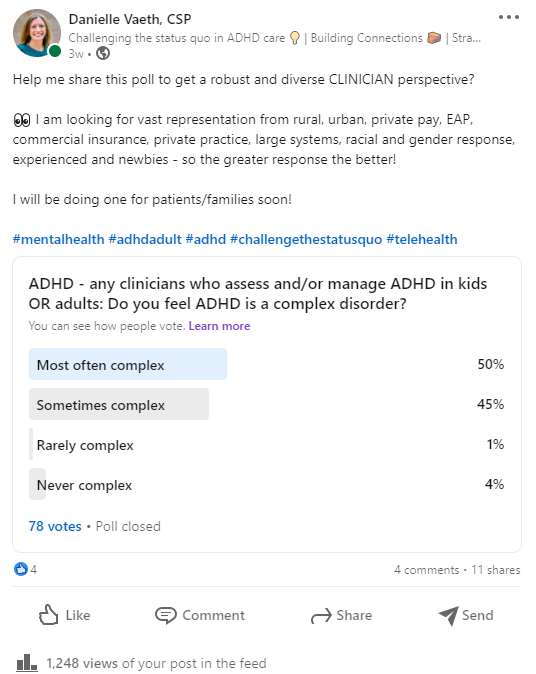
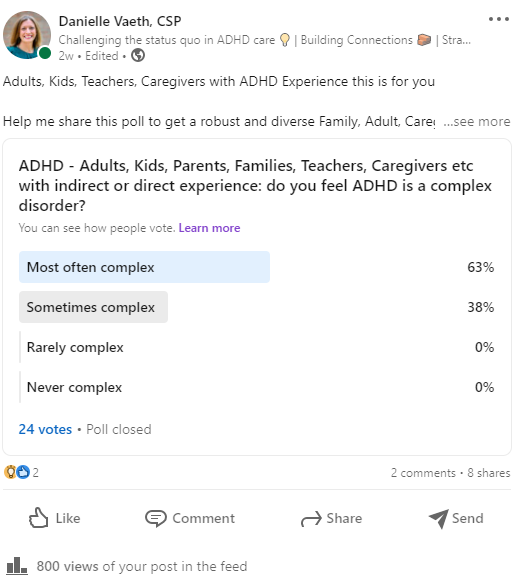
Since the meeting, I felt it important to conduct a survey of clinicians and of those with ADHD. I asked the following question via LinkedIn: Is ADHD a complex disorder? The results were consistent with the Consortium. 95% of the clinical group and 100% of the patient/caregiver group said that it is most often complex with over 50% in each group reporting ADHD as such.
And what did some of the providers have to say about this complexity?
One psychiatrist stated: “Psychiatry is highly subjective, and the prognosis is directly related to accurate diagnosis and the practitioner you see; ADHD is a case in point. “
Additionally, two psychiatrists added that: “ADHD is both under and over-diagnosed. Whether you are assessing and managing children or adults, they each have their own unique challenges.”
“In children, schools and media tend to gravitate towards a diagnosis that is on-topic even trendy, to help get services to improve the child’s experience,” stated a child neurologist.
“In adults, there is retrospective bias, where adults many times will underreport retrospective self-ratings from childhood, making the work of assessing adults a bit like reading tea leaves,” wrote one adult psychiatrist.
A new path forward
I believe that by educating providers on the tools and evidence for assessing ADHD, treatment optimization, and long-term outcome improvements, the future will continue to brighten. I see a day when all clinicians and caregivers of those with ADHD are well informed of the nuances of this complex, chronic, lifelong condition to improve the outcomes for those struggling with hyperactivity, attention, and impulse control issues.
Moreover, the ADHD Expert Consortium believes in payment parity and adding objective data from efficient, low-cost tools like Qbtech’s QbTest, an FDA-cleared test that can be used in the clinic with the help of ADHD mental health care workers. I believe that providing clinicians and their patients with robust, individualized, validated data, and reports helps open conversations and provide education and understanding as to where to go next when it comes to diagnosis and longitudinal chronic care management of ADHD. Furthermore, the group believes that clinicians should be reimbursed fairly to improve the clinical practice guidelines and access for patients in rural and urban areas across the country.
Finally, as a fellow advocate of using objective and evidence-based measures in improving ADHD care, I would greatly appreciate your show of support by reviewing and signing the consensus statement, which you can do so openly or anonymously.
